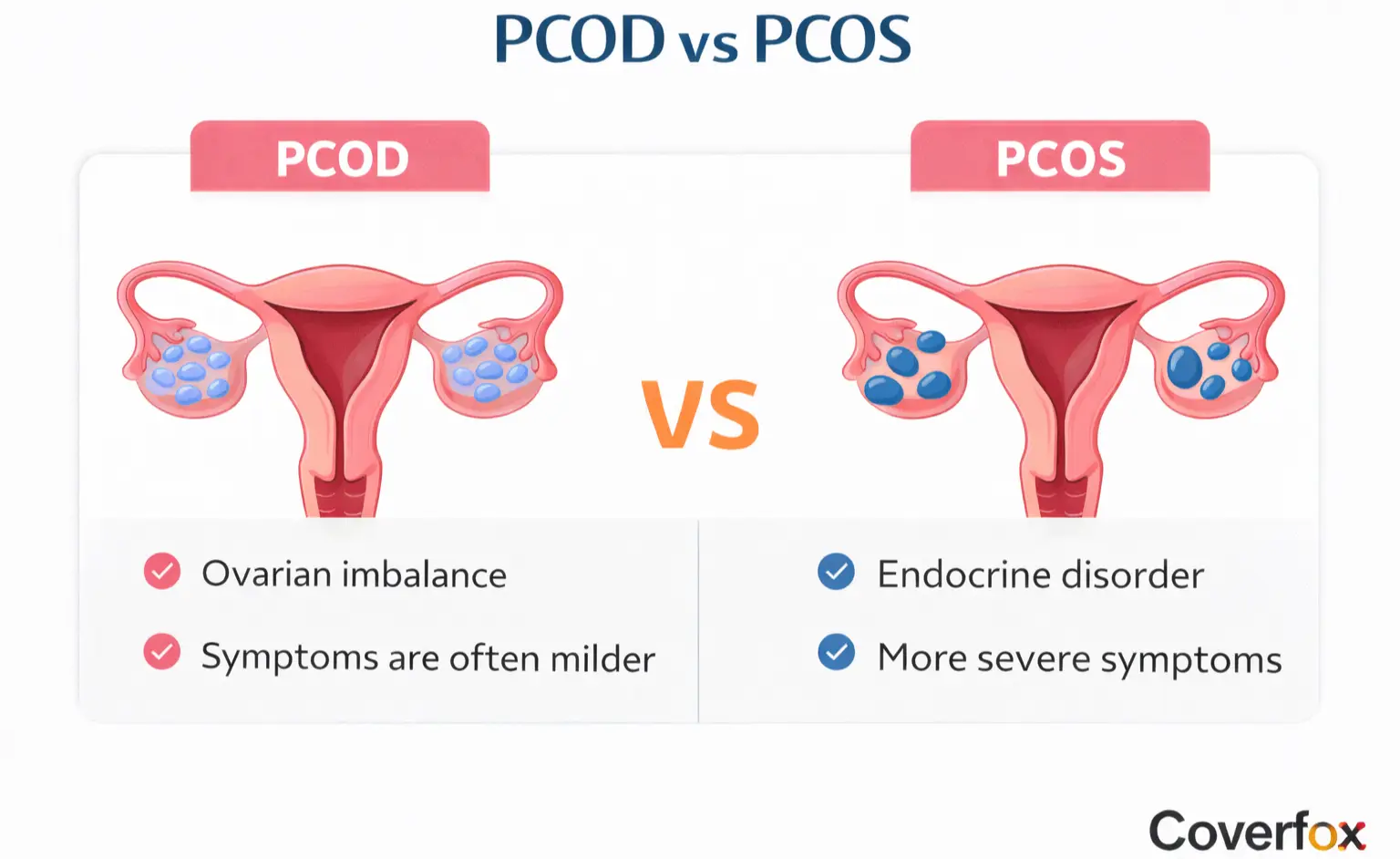
PCOD and PCOS are common hormonal conditions that affect women’s reproductive health but differ in severity, causes, and long-term health impact. While PCOD is usually linked to lifestyle factors and causes mild, manageable ovarian issues, PCOS is a chronic endocrine disorder associated with insulin resistance and metabolic risks.
PCOD and PCOS represent two distinct yet often confused conditions affecting women's reproductive health. They differ primarily in severity, hormonal impact, and systemic effects, and the PCOS and PCOD full forms denote 'Polycystic Ovarian Disease' and 'Polycystic Ovary Syndrome', respectively. Accurate diagnosis guides effective management, particularly relevant for health insurance coverage under comprehensive policies available.
What is the PCOD Problem?
PCOD, or Polycystic Ovarian Disease, is a condition that is caused by the ovaries producing immature or partially mature eggs in numerous small cysts. This hormonal disequilibrium interferes with normal ovulation, resulting in abnormal menstrual cycles. The main causes of PCOD are lifestyle, genetics, and insulin resistance, which affects up to 20% of women in India.
What are the Key Symptoms of PCOD?
Symptoms of PCOD and PCOS that are common to PCOD include:
Abnormal menstruation often results in significant or prolonged blood loss.
Abdominal-peripheral mild weight gain.
Marginal androgen increases acne and oily skin.
Abnormal growth of facial or body hair (hirsutism).
Problems with conception, but ovulation is intermittent.
These symptoms manifest slowly in late teens or early twenties.
What is the PCOS Problem?
PCOS, or Polycystic Ovary Syndrome, is a metabolic and endocrine condition in which the ovaries produce too many androgens, to the point of not releasing eggs at all. The cysts build up without bursting, and there is insulin resistance in various organs. According to the National Institutes of Health (NIH), the syndrome affects 5–18% of women in the world, with risks of diabetes and cardiovascular problems.
Diagnosis is based on Rotterdam criteria, including two out of three features: abnormal ovulation, elevated androgens, and polycystic ovaries on ultrasound.
What are the Key Symptoms of PCOS?
Extremely irregular or missing periods (amenorrhoea).
Considerable weight gain and obesity of unexplained origin.
Deep-seated hirsutism, acne, and male-pattern baldness.
Darkening of skin (acanthosis nigricans) of the neck or groin.
Mood disorders, infertility, and sleep apnoea.
The long-term effects are type 2 diabetes and the risk of endometrial cancer.
Symptoms of PCOD and PCOS: Overlap and Differences
Both conditions share hormonal roots, causing PCOD vs. PCOS confusion:
| Symptom | PCOD | PCOS |
|---|---|---|
| Menstrual Irregularity | Mild, cycles present | Severe, often absent |
| Weight Gain | Moderate | Obesity common |
| Hair Growth | Mild hirsutism | Severe androgen signs |
| Fertility Impact | Manageable | High infertility risk |
| Systemic Effects | Ovarian-focused | Metabolic syndrome |
PCOD vs PCOS: What’s the Difference?
The fundamental distinction between PCOS and PCOD lies in the pathology: PCOD is caused by functional ovarian cysts due to immature eggs, and they are reversible with lifestyle modifications. PCOS is a hereditary, hyperandrogenic, and insulin-resistant syndrome that cannot be treated and continues throughout life.
PCOD influences ovarian balance in a mild manner; PCOS interferes with endocrine activity in the body.
Detailed Comparison between PCOD & PCOS
Key distinctions appear in this table:
| Aspect | PCOD | PCOS |
|---|---|---|
| Full Form | Polycystic Ovarian Disease | Polycystic Ovary Syndrome |
| Causes | Lifestyle, genetics | Genetic, insulin resistance |
| Severity | Mild, common | Severe, complex |
| Ovulation | Irregular but present | Absent or rare |
| Complications | Limited | Diabetes, heart disease |
| Curability | Lifestyle reversible | Managed, not cured |
| Prevalence | 20–25% women | 5–15% women |
What are the Treatment Options for PCOD and PCOS?
Treatment and monitoring for PCOS and PCOD are distinct, despite the fact that both conditions share many symptoms.
Treatment Options For PCOD
Lifestyle Management
Hormonal Regulation
Medical Support & Monitoring
Long-Term Risk Reduction
A diet low in refined sugars and high in fibre and low in glycaemic index foods helps keep insulin and hormone levels stable. To improve ovarian health, you need to get at least 30 minutes of exercise every day. This can include things like brisk walking, yoga, or strength training. For many women, losing 5 to 10% of their body weight will bring back their periods.
Doctors use combined oral contraceptives to help patients manage their menstrual cycles and treat their acne. Women who cannot take oestrogen-based pills should use cyclic progesterone as their recommended treatment.
The minimal medication needs require physicians to track their patients' progress through pelvic ultrasounds and hormone tests. Patients who maintain a regular lifestyle pattern usually achieve positive results.
People who keep their weight in check and work out regularly are less likely to have metabolic health problems.
Treatment Options For PCOS
To treat PCOS, you need to keep your body weight in a healthy range, follow a low-carb diet, and do regular exercise. The treatment results show that making changes to your lifestyle can help with insulin resistance.
Medical Treatment
Hormonal & Reproductive Care
Long-Term Monitoring
The treatment of insulin resistance receives support through the use of metformin. Anti-androgens such as spironolactone provide treatment for both acne and excessive hair growth. The prescription medications clomiphene and letrozole serve as fertility treatment drugs that doctors use to help their patients achieve ovulation.
Women who want to avoid pregnancy use oral contraceptives to control their menstrual cycles. The infertility treatment requires custom solutions which depend on the patient's ovulation cycles.
PCOS patients need regular diabetes tests, cholesterol level assessments, and blood pressure monitoring because their condition increases their risk for metabolic diseases.
Also Read:
Disclaimer: This article is intended for informational purposes only and should not be considered medical advice, diagnosis, or treatment. PCOD and PCOS symptoms, severity, and treatment options may vary from person to person. Always consult a qualified gynaecologist or healthcare professional for personalised medical guidance. Insurance coverage, inclusions, and exclusions may differ by insurer and policy terms. Readers are advised to review policy documents carefully before making insurance-related decisions.
FAQs on PCOD vs PCOS
What is the difference between PCOD and PCOS?
Reversible ovarian cysts, primarily caused by lifestyle and hormonal disruptions, characterise PCOD. PCOS is a chronic syndrome that is characterised by serious hormonal imbalances, insulin resistance, and metabolic problems that affect various systems. These can be diagnosed early and adequately managed.
Are PCOD and PCOS similar in their symptoms?
The two conditions are characterised by irregular periods, weight gain, acne, and hirsutism because they have similar hormonal causes. The symptoms of PCOS become much more pronounced, with the appearance of severe androgen overload, infertility, obesity, and darkening of the skin. A clinical assessment helps explain the level of severity.
Are PCOD and PCOS the same thing?
No, PCOD is a disorder that is limited to ovarian malfunction and can be corrected well by lifestyle changes. PCOS is a complicated endocrine disorder that affects the health of the entire body and has a lifetime of monitoring needs. Medical prescriptions distinguish between these.
Can PCOD develop into PCOS?
In some cases, untreated PCOD leads to the development of PCOS due to unchecked insulin resistance. Regular observation through early weight control and metabolic screening prevents this transition. The interventions based on lifestyle are most effective at an early age.
What are the differences between the PCOD and PCOS treatments?
Diet, exercise, and weight loss are the sole interventions in PCOD management, which typically restore normal cycles within a few months. The treatment of PCOS incorporates both medications, such as metformin to control insulin levels and hormonal therapies, and long-term lifestyle modifications. Professional management supports individual procedures.
.webp)
 in Insurance.webp)