Low haemoglobin affects oxygen supply in the body, leading to fatigue, breathlessness, dizziness, and reduced physical capacity when levels fall below the normal range.
Common causes of low haemoglobin include iron deficiency, vitamin B12 or folate deficiency, blood loss, and chronic medical conditions, with diagnosis confirmed through blood tests like CBC and ferritin levels.
Treatment depends on severity, ranging from dietary changes and supplements to medical intervention such as injections or blood transfusions in critically low cases.
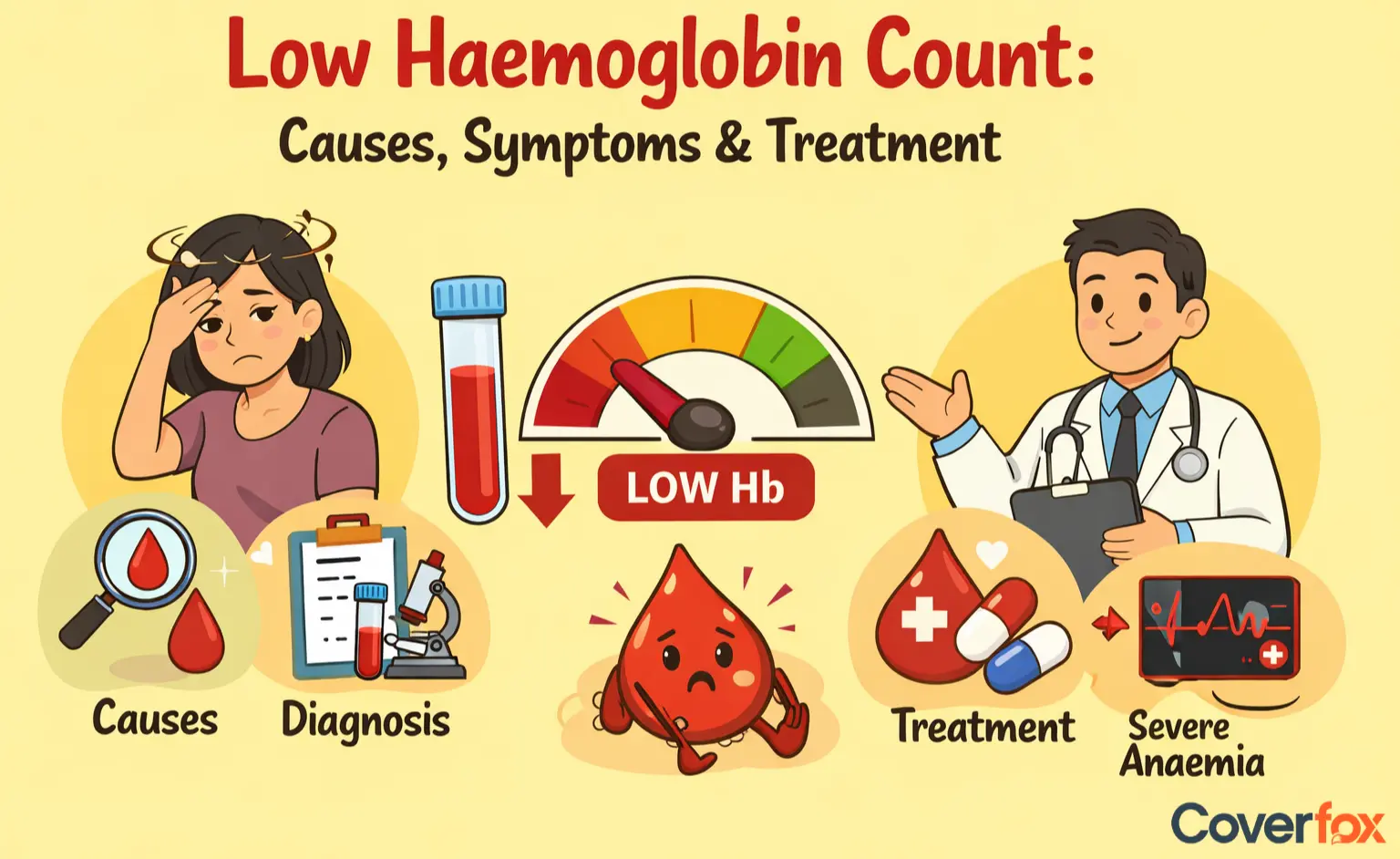
Low haemoglobin, affecting millions worldwide, often reveals itself through persistent fatigue that disrupts even simple daily tasks. This essential protein in red blood cells transports oxygen from lungs to tissues—when levels fall below 12 g/dL for women or 13 g/dL for men, organs receive an insufficient supply, triggering widespread symptoms like pale skin, shortness of breath, dizziness, cold extremities, and rapid heartbeat. Common causes include iron deficiency (accounting for 60% of cases), vitamin B12 or folate shortages, chronic blood loss from heavy periods or ulcers, and underlying conditions like kidney disease or thalassaemia.
periods or ulcers, and underlying conditions like kidney disease or thalassaemia. Diagnosis starts with a complete blood count (CBC) test measuring haemoglobin alongside ferritin for iron stores, often followed by stool tests for occult bleeding. Treatment varies by severity: mild cases respond to oral iron supplements (100-200mg elemental iron daily) paired with vitamin C-rich foods for absorption, while B12 injections or folate tablets address nutritional gaps; severe anaemia may require blood transfusions or erythropoietin therapy, with dietary emphasis on spinach, lentils, and red meat yielding improvements in 70% of mild cases within 3 months.
What is Haemoglobin?
Normal Haemoglobin resides in red blood cells, binding oxygen in the lungs before delivering it to tissues throughout the body. Low oxygen supply causes fatigue and slows bodily functions, while this iron-rich protein also imparts the blood's red colour.
WHO Normal Haemoglobin Ranges
Men
Women
Children (6-12 yrs)
Pregnant women
13.8-17.2 g/dL
12.1-15.1 g/dL (non-pregnant)
11.5-15.5 g/dL
11.0-14.0 g/dL (adjusted for trimester)
Levels vary by age, sex, pregnancy, altitude (>3,000m reduces by 1-2 g/dL), and smoking (elevates 1-2 g/dL). Single readings need trends for diagnosis—consult CBC tests for accuracy.
What Happens If Haemoglobin is Low?
Low haemoglobin means red blood cells cannot carry enough oxygen. The body tries to cope by increasing breathing or heart rate. The person may feel weak while walking short distances. Occasionally, there is trouble concentrating.
In slow-developing cases, people adapt without noticing until the symptoms become too strong to ignore. The effects manifest more quickly and intensely if the condition declines significantly. The WHO notes that anaemia affects a significant portion of the global population, particularly women and children, highlighting the importance of early detection.
Critically Low Haemoglobin Level?
Doctors often treat levels under 8 g/dL as serious. When it falls below 5 g/dL, it shifts into an emergency. At this stage, oxygen delivery becomes too low for organs. Such cases may bring confusion, severe breathlessness, and even risk of organ failure. Immediate medical treatment is needed because the body cannot manage on its own when the normal haemoglobin levels drop this far. Critical Thresholds:
Haemoglobin Level less than 8 g/dL
Haemoglobin Level less than 5 g/dL
Haemoglobin Level less than 7 g/dL pregnant
Symptomatic (confusion, tachycardia)—hospital admission, transfusions if symptomatic
Life-threatening (shock, organ hypoxia)—immediate IV iron/EPO + blood transfusion
A haemoglobin level less than 7 g/dL during pregnancy is considered critically low and may indicate severe anemia, requiring immediate medical attention.
Symptoms are extreme breathlessness, chest pain, and altered consciousness signal crisis. Context matters—acute drops (post-bleeding) are worse than chronic; comorbidities (heart/kidney disease) lower tolerance to 9 g/dL. Always correlate with ferritin and MCV for the root cause.
What are the Causes of Low Haemoglobin?
Low haemoglobin can appear due to many different reasons. According to the NIH, common causes include:
Low iron intake or poor absorption
Lack of vitamin B12 or folate
Blood loss from injury, surgery or heavy menstrual flow
Long-term diseases, such as kidney conditions
Bone-marrow issues that reduce red blood cell production
Certain medicines are used for long periods
These problems reduce haemoglobin in the human body and affect how oxygen reaches tissues.
What are the Symptoms of Low Haemoglobin?
Some symptoms appear early; others appear later. Many people notice more than one sign at the same time. The haemoglobin deficiency symptoms usually include:
Constant tiredness
Weakness when doing basic activity
Pale or yellow-shaded skin
Breathlessness
Faster heartbeat than usual
Feeling cold in the hands and feet
Dizziness or mild confusion
These symptoms do not always point to one cause, but they show that the oxygen level in the body may not be enough.
How are Haemoglobin Levels Tested?
A Complete Blood Count test, often called CBC, is recommended by the WHO to check haemoglobin. A small blood sample from a vein is taken. The test also shows red cell and white cell numbers. Occasionally, the doctor adds iron tests or vitamin level tests if the cause is not clear.
People with long-term health conditions may need repeated blood tests over months to watch for sudden drops.
Low Haemoglobin Treatments
Treatment for low haemoglobin (anaemia) depends strongly on the underlying cause. While mild cases can often be improved with dietary changes and supplements, more severe or complex cases may need deeper medical intervention.
Common Approaches to Treat Low Haemoglobin
Iron tablets or injections
Increase in iron-rich foods
Vitamin B12 or folate treatment
Medication that helps bone marrow produce more red blood cells
Blood transfusion in severe cases
Managing chronic diseases that cause the problem
WHO emphasises that most cases of anaemia, especially iron deficiency, are preventable and treatable with proper diet, supplementation, and medical care.
Conclusion
Low haemoglobin does not come from one reason alone. It can show up due to a lack of iron, blood loss, or a deeper medical issue. Knowing the critically low haemoglobin level can help judge when the condition moves into unsafe territory. People with chronic health concerns must track levels more often, since quick drops can create sudden weakness.
Understanding typical symptoms and how testing works makes the condition easier to manage. Treatment varies widely, from supplements to transfusions, depending on what led to the fall. Awareness also helps when reviewing health insurance plans, as some conditions require longer management and repeated tests.
Disclaimer: This content is for general informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional for diagnosis, treatment, or concerns about low haemoglobin or related health conditions. Insurance coverage and benefits may vary depending on the policy.
Read More:
FAQs on Low Haemoglobin Levels
What is considered a low haemoglobin level?
A value falls below the normal haemoglobin level range. Values below 8 g/dL are usually treated more urgently.
How is low haemoglobin diagnosed?
A CBC test is one such test. Doctors may add iron studies or vitamin tests.
When should I consult a doctor for low haemoglobin?
If symptoms continue for days or breathing becomes difficult, a doctor should examine the case.
Does having low haemoglobin mean I have anaemia?
Often, the answer is yes, but the cause still requires verification.
Can lifestyle changes improve haemoglobin levels?
Dietary changes, improved nutrition, and the treatment of underlying issues can be beneficial in mild cases.
.webp)
 in Insurance.webp)