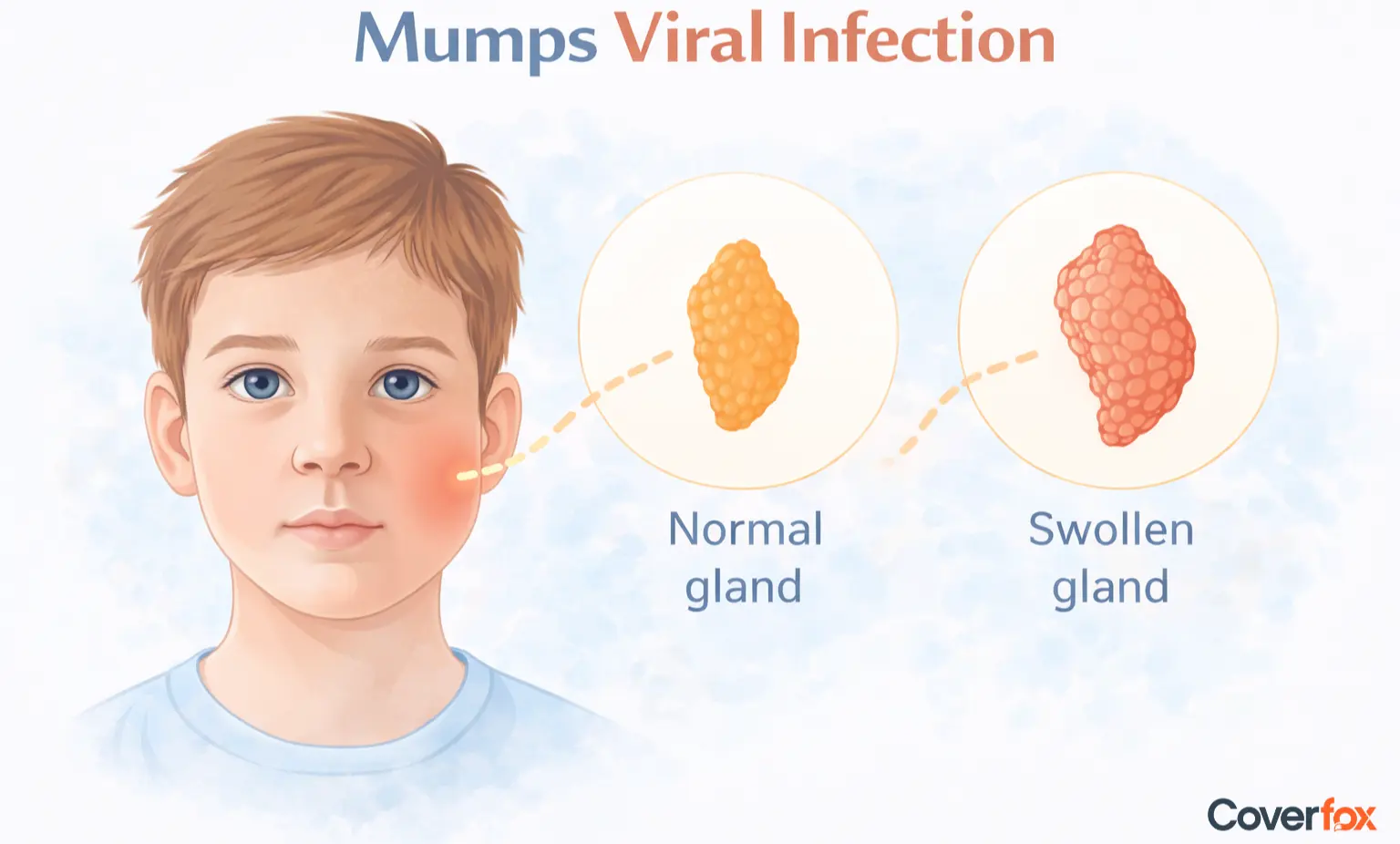
Mumps constitutes a highly contagious viral disease primarily affecting salivary glands, particularly the parotids. It is caused by the mumps virus, which spreads through respiratory droplets and close contact with an infected person, and it typically presents with painful facial swelling, fever, and fatigue. Prevention of mumps disease relies on vaccination, while understanding transmission proves crucial for outbreak control.
What is Mumps Viral Disease?
Mumps is caused by the paramyxovirus, which first multiplies in the upper respiratory system before attacking the salivary glands. The virus spreads through saliva and respiratory droplets, establishing an infection 12–25 days after exposure. Parotitis characterises 70%–90% of symptomatic cases, with one-third remaining asymptomatic despite contagiousness.
The disease occurs worldwide, though vaccination programs have reduced its incidence by 99%, according to the Centres for Disease Control and Prevention (CDC). Humans serve as the sole natural reservoir.
Mumps symptoms in adults mirror childhood presentation but carry higher complication risks. Swollen parotid glands create tender jawline swelling lasting 7-10 days. Adults experience more pronounced fever, headaches, and muscle aches along with orchitis in 25–50% of postpubertal males. Immunity from prior infection or vaccination offers lifelong protection. Transmission peaks 2 days pre-symptom onset through 5 days post-parotitis, and adults in close-contact settings like offices face elevated exposure.
What are the Causes of Mumps Disease?
Mumps, caused by the Rubulavirus species within the Paramyxoviridae family, spreads via:
Direct contact with infected saliva occurs during kissing or sharing utensils.
Coughing, sneezing, or talking can release airborne droplets of the virus.
Contaminated surfaces can harbour viable viruses for hours.
The virus enters the body through the nose or mouth via respiratory droplets and initially multiplies in the upper respiratory tract. It then spreads through the bloodstream to the salivary glands and other tissues, leading to inflammation and swelling. Incubation spans typically 16–18 days, with viral shedding commencing pre-symptomatically. Crowded environments accelerate community spread.
What are Mumps Disease Symptoms?
Mumps symptoms usually show their first signs after the incubation period ends, and they become worse during a three-day period before symptoms start to get better.
Prodrome Phase
Parotitis Phase
Systemic Symptoms
When to Seek Medical Attention
The first symptoms that appear during this stage include fever at 39°C and malaise, together with headache, muscle aches and loss of appetite, which continue for one to two days. The initial signs of the condition, which appear at the beginning of the illness, show only mild symptoms that mimic a standard viral infection.
The next stage of the disease starts with painful swelling that affects one salivary gland, which occurs in 75% of cases, but the condition can progress to affect both glands within 1–2 days. The swelling reaches its maximum size on the third day, which creates challenges for the patient when they try to chew or swallow food.
The body experiences fatigue together with body aches that continue for a period of 7 to 10 days. Adult patients experience more intense symptoms, which include testicular pain and swelling, together with abdominal pain and only infrequent neurological side effects.
Emergency medical help needs to be obtained when someone experiences a severe headache, along with neck stiffness, persistent vomiting, or a high fever. Mumps symptoms in adults intensify with testicular pain (orchitis), abdominal discomfort (pancreatitis), or neurological signs.
How Long Does Mumps Disease Last?
| Complication | Incidence | Sequelae |
|---|---|---|
| Orchitis | 25-35% adult males | Rare infertility |
| Meningitis | 1-10% | Full recovery usual |
| Pancreatitis | 4% | Self-limiting |
| Deafness | 1:20,000 | Permanent |
Mumps Complications
Orchitis
Oophoritis
Meningitis
Pancreatitis
Deafness
Occurs in up to 30% of post-pubertal males, making it one of the more common complications in adults. However, bilateral involvement and permanent sterility are rare (less than 1%).
Affects around 5% of post-pubertal females and is less common than orchitis, with long-term fertility issues being uncommon.
Seen in approximately 10–15% of cases, usually as aseptic meningitis. It is relatively common among complications, but typically mild and self-limiting.
An uncommon complication that usually presents with temporary enzyme elevation and abdominal discomfort, resolving without lasting damage.
Extremely rare (around 0.005%), typically unilateral, but may be permanent in very few cases.
Diagnosis of Mumps Disease
Diagnosis usually begins with clinical suspicion based on characteristic parotid swelling and fever.
Viral PCR (Buccal/Throat Swab)
Serology (IgM and IgG Antibodies)
Viral Culture
Imaging (Ultrasound/MRI)
This is the best test to confirm the diagnosis at first, especially in the early stages of the illness. With a sensitivity of 85–90%, PCR is most accurate when performed within the first few days of gland swelling.
Serum IgM antibodies are typically detectable within the first week of symptom onset, while IgG seroconversion appears by the third week. Serology is useful when PCR is unavailable or when diagnosis is delayed.
Although specific, viral culture from saliva takes 5–7 days and is rarely used for routine diagnosis due to the slow turnaround time.
Ultrasound is used when the diagnosis is uncertain or to confirm parotid gland involvement. MRI is reserved for suspected complications such as meningitis, encephalitis, or other central nervous system involvement.
Who is at Risk of Mumps Disease?
Unvaccinated individuals face the highest vulnerability due to a lack of protective immunity.
Children aged 5–9 years
Adolescents and Young Adults
Immunodeficient Patients
Pregnant Women
In communities with low vaccination coverage, children remain susceptible because they may not have received complete MMR doses, creating immunity gaps.
Those living in hostels, colleges, or military settings face a higher risk due to close-contact exposure, which facilitates rapid viral transmission. Decreasing immunity over time may also play a role.
Individuals with weakened immune systems may have reduced vaccine responses or declining immunity, making them more prone to infection and complications.
Although rare, infection during pregnancy, especially in the first trimester, may increase the risk of miscarriage due to systemic viral effects.
How to Prevent Mumps Disease?
The most reliable method is MMR (Measles, Mumps, Rubella) vaccination:
Vaccination Schedule
Standard Vaccine
Outbreak response
The first dose is typically given at 9–12 months of age (as per national schedules), and the second dose at 15–18 months or 4–6 years. Two doses provide approximately 88% (first dose) to 95% (second dose) effectiveness.
The single-antigen mumps vaccine has been discontinued; the combined MMR vaccine is the recommended and widely used option.
In high-risk settings during outbreaks, a third MMR dose may be advised to boost immunity and significantly enhance protection.
How Safe is the MMR Vaccine?
The MMR vaccine maintains an established safety profile across hundreds of millions of administered doses worldwide. Common mild reactions include fever in 5-15% of recipients and rash in approximately 5%, occurring 7-12 days post-vaccination due to immune response activation.
Serious side effects are still very rare. Anaphylaxis happens in 1 out of every million doses, and aseptic meningitis is linked to certain strains in 1 out of every 300,000 doses, according to NIH. Extensive epidemiological studies involving millions consistently demonstrate no association between MMR vaccination and autism spectrum disorders.
The live weakened virus grows in the respiratory system of healthy people without spreading throughout the body, providing long-lasting protection against measles, mumps, and rubella. Two-dose schedules achieve 88-95% effectiveness, representing the cornerstone of mumps prevention.
How to Prevent the Spread of Disease?
Effective containment measures are essential to reduce transmission, as mumps spreads easily through respiratory droplets and close contact. Below are preventive measures:
Isolation for 5 days after parotitis onset
Droplet precautions
Exclusion from school or work
Surface disinfection and hand hygiene
Infected individuals are most contagious around the time of gland swelling. Staying isolated during this period significantly reduces the risk of spreading the virus to others.
Masks should be worn, and people should maintain distance from cases who are within 1 metre because this practice prevents respiratory droplets from being released during coughing, sneezing, and talking.
People should stay away from crowded places until their swelling decreases because such action measures their risk of close contact and helps prevent multiple people from becoming infected.
The combination of washing shared surfaces and teaching proper handwashing techniques helps to decrease the risk of people becoming infected through contact with contaminated objects, which are known as fomites.
How to treat Mumps Disease?
Mumps disease treatment remains entirely supportive, as no specific antivirals target the paramyxovirus effectively. Healthcare providers recommend ibuprofen or paracetamol for pain relief and fever management, avoiding aspirin due to Reye's syndrome risk in viral infections.
Appropriate hydration prevents salivary gland dehydration, while soft foods like soup and yoghurt minimise parotid strain during chewing. Cold compresses applied externally reduce glandular swelling and oedema through vasoconstriction. Bed rest continues until the fever resolves completely, typically spanning 7-10 days from symptom onset.
Hospitalisation becomes necessary for complications such as orchitis, pancreatitis, or meningitis rather than uncomplicated parotitis. Intravenous fluids support severe cases alongside monitoring for secondary bacterial infections. In such situations, having an appropriate health insurance coverage can help manage the financial burden of hospital stays, specialist consultations, and diagnostic investigations.
Key Takeaways
Mumps is a highly contagious viral infection affecting the salivary glands, with adults facing a higher risk of complications such as orchitis, meningitis, and pancreatitis. Two doses of the MMR vaccine provide 88–95% protection and remain the most effective way to prevent mumps and its complications. Early diagnosis, isolation for five days after gland swelling, and supportive care are essential to control spread and ensure safe recovery.
Also Read:
Disclaimer: This article is intended for informational purposes only and does not substitute professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for medical concerns. Coverage for mumps-related hospitalisation and complications depends on policy terms, conditions, and insurer guidelines.
Frequently Asked Questions on Mumps Disease
Does mumps constitute a viral disease?
Mumps qualifies as a viral disease caused exclusively by the paramyxovirus. Bacterial agents do not produce characteristic parotitis. Vaccination prevents nearly all clinical infections.
Can mumps spread by touch?
Mumps spreads primarily through respiratory droplets, not casual touch. Fomites contaminated by saliva transmit rarely. Handwashing disrupts indirect spread effectively.
How long does mumps last in adults?
It spans 10–14 days, from prodrome to parotitis resolution in adults. Fatigue persists for weeks; orchitis extends recovery 3-4 weeks.
Is isolation required for mumps?
Isolation remains mandatory for five days post-parotitis onset per CDC guidelines. This phase contains transmission during peak viral shedding. Return follows clinical improvement.
What is the infectious period of the mumps?
Infectious period spans 12 days: 2 days pre-symptom onset through 5 days post-parotitis plus a 5-day tail. Highest contagiousness coincides with glandular swelling.
.webp)
 in Insurance.webp)