Tubectomy (tubal ligation) is a permanent female sterilisation procedure that blocks the fallopian tubes to prevent pregnancy, with about 99% effectiveness. It is usually done laparoscopically or after childbirth, has low complication rates, and does not affect periods or hormones, but reversal is difficult and often unsuccessful, making proper counselling essential before opting for it.
Women choose permanent contraception like tubectomy after careful consideration of family completion or health contraindications for future pregnancies. This surgery has a failure rate of 1 person per 100 women, having a 99% success rate. (National Health Mission)
Tubectomy Procedure Reality
Laparoscopic
Minilap
Complication Rate
20-30 min under general anaesthesia; 2 small abdominal incision
10-15 min local anaesthesia; abdominal band/tube clipping
0.5-2% (infection, bleeding, ectopic risk); 1/1,000 need re-operation [WHO data]
Tubectomy Eligibility
As per government norms, women aged above 22 years with at least two living children are eligible for tubectomy. A mandatory 72-hour cooling-off period is required between counselling and the procedure to ensure informed decision-making.
Tubectomy reversal is expensive (approximately ₹1–2 lakh) and has a success rate of less than 50%, making the procedure largely permanent. Therefore, detailed counselling about irreversibility, possible risks, benefits, and alternative contraceptive options is essential before obtaining informed consent.
What is Tubectomy Operation?
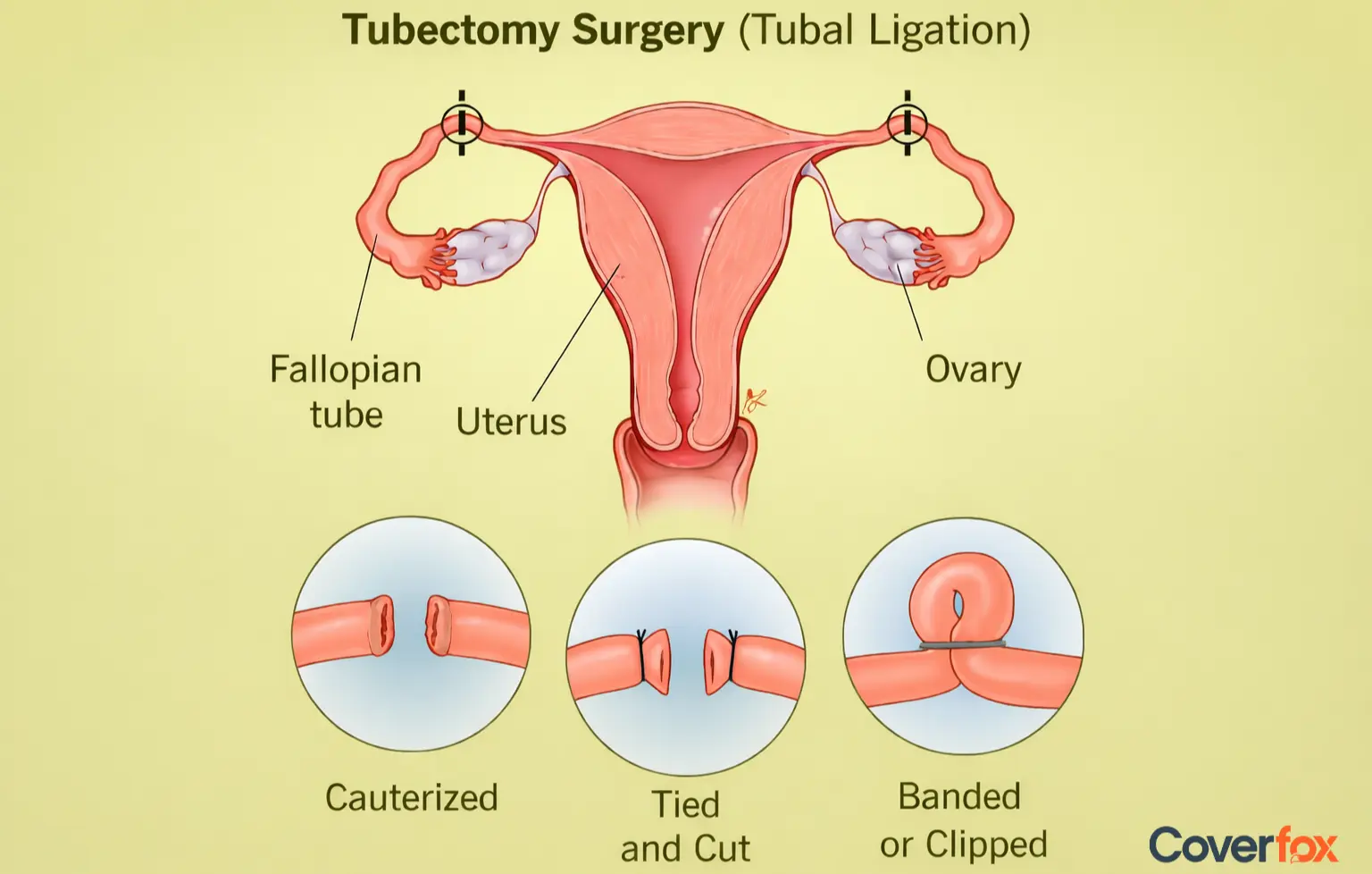
A tubectomy, or tubal ligation, is a permanent procedure where the fallopian tubes are cut, tied, or sealed. This stops sperm from reaching the egg. The egg still forms each month, but it gets absorbed by the body. Tubectomy prevents pregnancy with a 99.5% long-term success rate, boasting a failure rate of just 0.5 per 100 women over 10 years, according to NIH and CDC data outperforming vasectomy's 99.9% efficacy in practice.
Doctors strategically time procedures for minimal risk: postpartum within 1–7 days of C-section (covering 70% of Indian cases where abdominal access is already available), interval laparoscopic 6 weeks post-delivery (preferred in 80% of scenarios), or concurrent with hysterectomies/caesareans for opportunistic sterilisation.
India performs 5.5 million annually (NFHS-5 data) with 1-2% complication rates, primarily ectopics at 1/1,000; failures stem from rare recanalisation (0.26%). Mandatory 72-hour counselling ensures informed consent for this permanent method, where reversal succeeds <40% at ₹1-2 lakh. The tubectomy meaning stays the same in all methods: a surgical block of the fallopian tubes that prevents future pregnancies.
Why is a Tubectomy Done?
Doctors recommend tubectomy primarily for two key reasons backed by global guidelines like ACOG and WHO.
Family Completion
Medical Contraindications to Pregnancy
Women opt for tubectomy once their family is complete, seeking permanent contraception after informed counselling on alternatives—the only universal indication per ACOG, as it eliminates future fertility with 99.5% efficacy.
High-risk conditions like severe cardiopulmonary disease, renal issues, or pregnancy complications (e.g., BRCA mutations raising ovarian cancer risk by preventing future pregnancies) warrant tubectomy; full salpingectomy reduces ovarian cancer by 42-78%.
What is the Difference Between a Vasectomy and a Tubectomy?
Vasectomy and tubectomy both achieve permanent sterilisation by blocking gamete transport, yet they target distinct reproductive organs with varying procedural complexity and recovery profiles.
Vasectomy interrupts the vas deferens—two thin tubes (30-40 cm long) carrying sperm from the testes to the urethra; a small scrotal incision severs/ligates them, preventing sperm in the ejaculate (still 2-5 ml semen volume).
Tubectomy occludes fallopian tubes (10-12 cm each), halting egg descent from the ovaries to the uterus; it requires abdominal access for clipping, cutting, or coagulation.
Procedure & Recovery Comparison of Vasectomy & Tubectomy
| Aspect | Vasectomy | Tubectomy |
|---|---|---|
| Duration | 10–20 minutes, local anesthesia | 20–45 minutes, general or local anesthesia |
| Incisions | One small scrotal incision (office-based procedure) | One or two abdominal incisions (often laparoscopic) |
| Recovery | 2–7 days; semen testing required after 3 months | 1–2 weeks; hospital stay may be required |
| Complications | 1–2% (hematoma, infection) | 0.5–2% (ectopic pregnancy, bleeding) |
Vasectomy proves simpler, safer, and reversible more often (50-70% vs. tubectomy's <50%), per ACOG guidelines.
What are the Types of Tubectomy and How Do They Work?
Below is a table showing three common types and basic details.
| Type | Method | Recovery Time |
|---|---|---|
| Laparoscopic Tubectomy | Two small cuts are made; a thin tube with a camera helps the doctor locate and seal the fallopian tubes. | Often around 1 week |
| Laparotomy | A larger incision is made on the abdomen, usually performed after childbirth or during other abdominal surgeries. | A few weeks |
| Mini-laparotomy | A small incision is made after vaginal delivery, and the fallopian tubes are tied soon after childbirth. | Around 1–2 weeks |
Laparoscopic tubectomy is common today, as it needs only small cuts. Carbon dioxide fills the abdomen to help the doctor see clearly.
Laparotomy is more extensive, often done with other major surgeries.
Mini-laparotomy is usually done within 24 hours of childbirth to avoid two separate surgeries.
What are the Side Effects of Tubectomy?
Most side effects of tubectomy are temporary and occur as the body recovers from surgery. Permanent side effects are rare. Most women recover well, but some may feel mild discomfort. Usual effects include:
Shoulder or neck pain
Abdominal cramps
Bloating
Tired feeling
Light nausea
Sore throat due to the anaesthesia tube
Less common problems may include:
Unusual vaginal discharge
Blood or pus from the cut
Fever
Pelvic pain
Swelling around the cut area
These may need a doctor's review.
Tubectomy: Post-surgery Care
Doctors usually share simple care steps for a smooth recovery. Some common advice includes:
Avoid a heavy load for a few weeks
Keep the cut clean and dry
Do not swim until the cut heals
Avoid alcohol or smoking for one day after surgery
Eat light food to avoid nausea
Use pain medicine only as the doctor advises
Many women walk slowly on the same day, but full activity may take a bit more time depending on the method used.
Effectiveness of Tubectomy
A laparoscopic tubectomy prevents pregnancy with 99.5% efficacy, carries defined risks, and has a failure rate of 0.5 per 100 women over 10 years, outperforming many other contraceptive methods.
Pregnancy Failure
Ectopic Pregnancy
First-Year Success
0.26-0.5% (recanalisation); cumulative 5-18/1,000 over 10 years
7.3/1,000 cases (36% of failures)—higher than the general population due to partial tubal patency
99% procedural completion rate
Rare failures (clips dislodging, spontaneous reconnection) underscore pre-op counselling on permanence. Monitor post-op for 3 months; ectopics present as abdominal pain/bleeding.
Recovery after Tubectomy
Recovery differs with each method. Laparoscopic patients often go home on the same day. Laparotomy may require a hospital stay for one or two days.
Menstruation
STI Protection
Sexual Activity
Periods continue after a tubectomy. One cycle may be delayed, but flow returns to usual in later months.
The operation does not protect against any sexually transmitted infection. Protection methods must still be used.
Sex may resume only after the doctor confirms proper healing.
Conclusion
Tubectomy remains one of the most used permanent birth control choices for women. The operation blocks the natural path of the egg and sperm, which stops pregnancy in almost all cases. Each person must speak with a medical expert to ensure the method suits their health. Recovery can be smooth when the care steps are followed.
For financial protection during surgery or later health needs, people often consider health insurance plans. Understanding the procedure, risks, and long-term implications helps individuals make informed family planning decisions. Proper counselling and post-surgery follow-up further ensure safety and peace of mind.
Also Read About:
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Tubectomy and other family planning procedures carry risks that vary per individual. Always consult a qualified healthcare provider before making decisions about surgery.
FAQs on Tubectomy
How long does a tubectomy surgery take?
Most surgeries take around 20–40 minutes, depending on the method and the patient’s health.
How soon can normal activities resume after tubectomy surgery?
Light movement may start within a day. Full activity may take one to two weeks, based on the type of tubectomy.
Will pain be felt after surgery?
Many women feel mild cramps or soreness for a few days. Pain medicine usually helps.
Does tubectomy cause weight gain?
Weight gain is not known to be caused by tubectomy. Weight changes usually happen due to lifestyle or other health reasons.
Do periods continue after a tubectomy?
Yes, most women have normal periods after the family planning operation, though one cycle may be delayed.
Are there any side effects of a tubectomy?
Mild pain, bloating, or tired feelings may occur. Severe symptoms are uncommon and need medical care.
Is tubectomy 100% safe?
Most surgeries are safe when done by trained doctors. Any surgery has some risks, which the medical team explains in advance.
Is tubectomy operation covered under health insurance?
Tubectomy operation is not covered by most health insurers, unless specifically mentioned. However, to be accurate, refer to your policy document.
.webp)
 in Insurance.webp)