Infertility affects both men and women and often requires advanced medical treatments that come with high costs. In India, most health insurance plans exclude IVF and assisted reproductive procedures, offering only limited coverage for diagnostics, consultations and treatment of underlying conditions. While select riders and corporate policies provide partial fertility benefits, coverage remains capped and conditional. Understanding policy terms, legal regulations and alternative financing options is essential for informed planning.
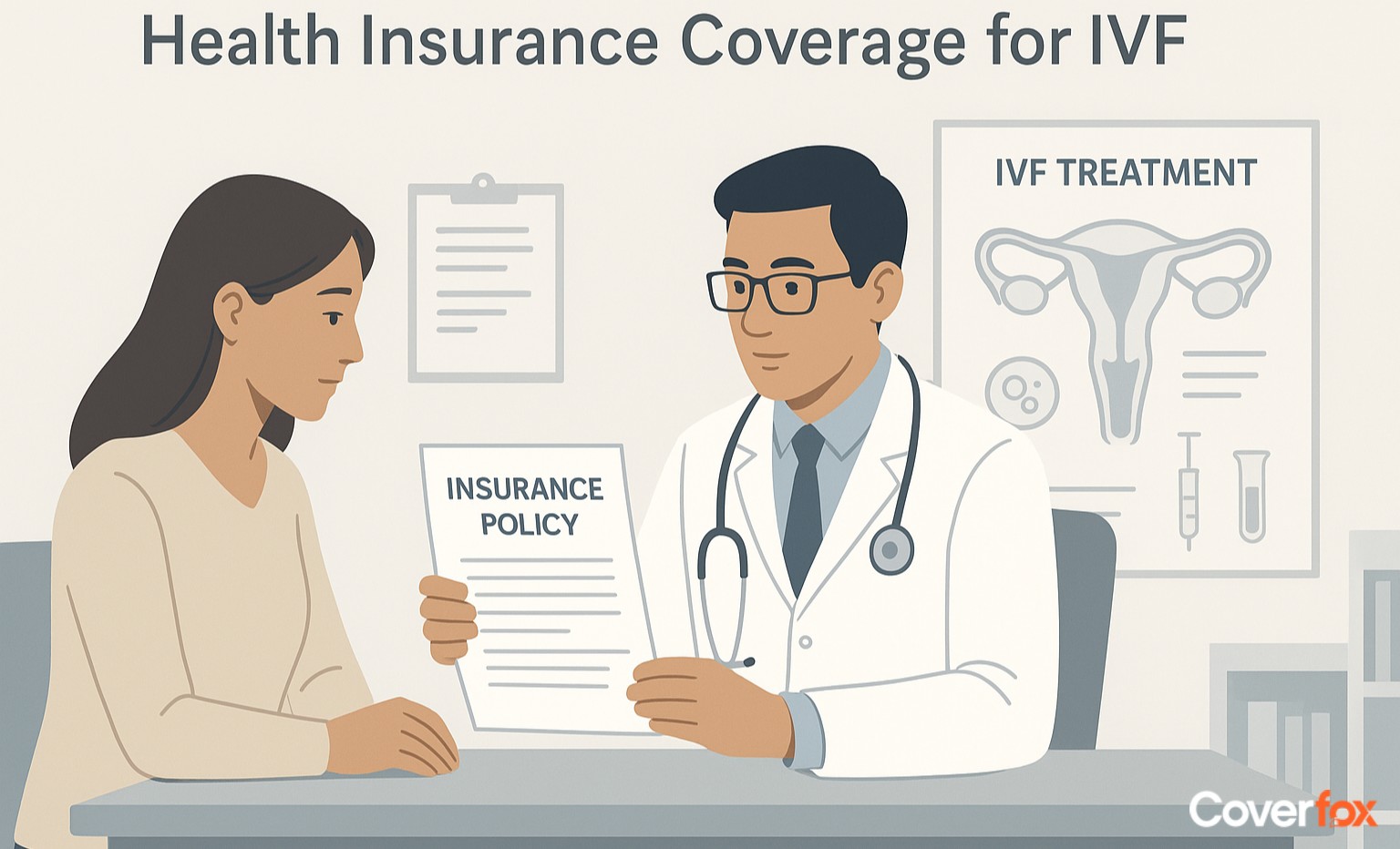
Infertility has been a growing cause of concern amongst the modern day couples. Not being able to procreate leads to mental stress and drives a wedge between the couple. Infertility refers to a condition where, even after a year of trying, not able to conceive a newborn. However, to tackle this, many infertility treatments have emerged today, but at an expensive cost. Health insurance kicks in here to help your wallet. Let us understand in detail about infertility treatments and health insurance through this article.
Understanding Infertility & Common Treatments
Infertility refers to the inability to conceive after 12 months of regular, unprotected intercourse, and it can arise from both male factors (low sperm count, poor motility, blockages) and female factors (ovulation issues, hormonal imbalance, blocked fallopian tubes, age-related decline). Modern fertility care includes several diagnostic and treatment options that help couples achieve pregnancy.
1. Common Fertility Diagnostics & Treatments
Understanding fertility diagnostics and treatments can help individuals and couples make informed decisions on their journey to conception, addressing a range of reproductive health challenges.
2. Diagnostics (Hormone tests, Ultrasound, Semen analysis)
Used to identify ovulation disorders, reproductive health issues and sperm quality problems.
3. Fertility Medications
Drugs like Clomiphene or hormonal injections stimulate ovulation or support egg development.
4. IUI (Intrauterine Insemination)
Processed sperm is placed directly inside the uterus to improve the chances of fertilisation.
5. IVF (In Vitro Fertilisation)
Eggs and sperm are combined in a lab, and a resulting embryo is transferred into the uterus.
6. ICSI (Intracytoplasmic Sperm Injection)
A single healthy sperm is injected into an egg, helpful in severe male infertility cases.
7. Egg Freezing (Oocyte Cryopreservation)
Eggs are harvested and stored at an early, healthy stage for future use, improving reproductive options later.
Current Health Insurance Rules for Infertility Treatment in India
In India, most standard health insurance plans exclude infertility treatments such as IVF, IUI and ICSI, considering them elective procedures. Some policies may cover basic diagnostics or specialist consultations, but treatment costs are usually out of pocket unless the customer opts for a premium plan that specifically includes limited fertility benefits.
A few insurers now offer add-ons or capped coverage, but availability remains selective. IRDAI guidelines require insurers to clearly state exclusions, though they do not mandate fertility treatment coverage. (Source - IRDAI)
What Health Insurance Typically Covers in Infertility Care?
Health insurance in India usually offers limited support for infertility, focusing mainly on diagnostics like ultrasounds, hormone tests and semen analysis, along with doctor consultations. Many policies also cover the treatment of underlying medical conditions that affect fertility, such as PCOS, fibroids, endometriosis, infections or thyroid disorders, and may include medically necessary surgeries that can help restore fertility.
Insurers may offer 50–70% coverage for certain supportive treatments, depending on the plan. Coverage varies by insurer, so comparing policy options is crucial for understanding what is included and excluded.
Fertility Insurance Riders & Specialised Plans
While infertility coverage is still limited in India, a few insurers and corporate health policies offer specific riders or benefits that support certain aspects of fertility care, usually with financial caps and conditions.
1. Infertility Treatment Rider
Offers limited coverage for fertility-related consultations, diagnostics, or select treatments, often capped per policy year.
2. IVF / Assisted Reproduction Rider
Provides partial reimbursement for IVF, IUI or ICSI procedures, typically available only with premium or corporate group plans.
3. Maternity with Fertility Add-on
Extends maternity coverage to include fertility treatments as an optional paid add-on.
4. Hormonal Therapy Coverage Rider
Covers prescribed fertility-related hormone medications and injections, subject to limits.
5. Laparoscopic Surgery Coverage
Includes medically necessary fertility-restoring surgeries like laparoscopy or hysteroscopy.
6. Egg Freezing or Fertility Preservation Rider
Covers egg or sperm freezing in select policies, usually for medical reasons and with strict eligibility criteria.
NOTE: These riders usually come with waiting periods, age limits, sub-limits and pre-authorisation requirements, making coverage partial rather than comprehensive.
Cost of Infertility Treatments & Why Insurance Matters
Infertility treatments can be financially demanding, with costs ranging from ₹1,00,000 to ₹4,00,000 per cycle, and multiple cycles are often needed for success. Since most health insurance plans offer limited or no coverage for advanced fertility procedures, these expenses are usually paid out of pocket. Even partial insurance support can significantly reduce financial stress and help couples focus on treatment rather than costs.
Government Policies & Legal Framework for Fertility Treatments in India
In India, the Assisted Reproductive Technology (Regulation) Act, 2021 governs fertility treatments like IVF, IUI and related procedures by regulating clinics and ART banks, requiring them to register, maintain standards and follow ethical protocols to protect patients and donors. (ICMR).
The law aims to bring transparency, patient safety and accountability to ART services, and is complemented by the Surrogacy (Regulation) Act, 2021, which prohibits commercial surrogacy and permits only altruistic arrangements with strict eligibility criteria for intended parents and surrogates. (https://artsurrogacy.gov.in/).
These regulations affect cost, access and legal obligations for clinics and patients by setting standards and oversight mechanisms, but do not mandate that health insurers must cover infertility treatments or ART procedures, leaving coverage decisions to individual insurers and policy terms.
Key Things to Check Before Buying Health Insurance for Infertility Treatment
Infertility treatments vary widely in cost and complexity, and not all health insurance policies offer the same level of support. Reviewing the fine print before choosing a plan can help you avoid gaps in coverage when you need it most.
Check whether the policy has specific eligibility criteria, such as a minimum sum insured of ₹5 lakh or more, to access fertility-related benefits.
Verify if infertility diagnostics like hormone tests, ultrasounds and semen analysis are covered.
Confirm which fertility procedures are included, such as IVF, IUI, ICSI or only supportive treatments.
Understand the waiting period, which can range from 2 to 6 years before claims are allowed.
Check whether fertility medications and hormone injections are included, as these can form a large part of treatment costs.
Look for relevant add-ons or riders that enhance fertility-related coverage.
Ensure pre-authorisation requirements are clear to avoid claim rejections.
Confirm any age restrictions that may apply to fertility-related claims.
Compare multiple insurers to understand differences in coverage scope and exclusions.
Alternatives When Insurance Does Not Cover Fertility Treatment
When health insurance does not cover fertility treatments, couples often need to explore alternative ways to manage the financial and emotional burden. Planning ahead and understanding available options can make treatment more accessible.
Fertility-specific loans from banks and NBFCs
EMI or instalment programmes offered by fertility clinics
Government hospitals and medical colleges offering low-cost IVF
Financial aid from NGOs, trusts or charitable institutions
Planned savings or dedicated fertility funds
Conclusion
While infertility is a growing concern amongst couples, ensuring that your health insurance covers treatments related to it, and planning ahead of time will make life a lot easier. Make sure to read your insurance policy document carefully before purchasing one, and understand inclusions and exclusions well. To get the best health insurance quotes from different insurers, you can very well rely on Coverfox.
Disclaimer: The information provided above is for general awareness purposes only and should not be considered as medical advice. Coverage, inclusions and exclusions may vary by insurer; always refer to the official policy document or consult your insurer for accurate and up-to-date details.
Read More About Health Insurance in India
FAQS on IVF & Health Insurance in India
Does health insurance in India cover infertility treatment or IVF procedures?
Most standard health insurance plans do not cover infertility treatments or IVF, though limited benefits may be available under select premium plans or riders.
Which infertility treatments are usually covered under health insurance?
Coverage of infertility treatments is generally limited to diagnostics, doctor consultations, treatment of underlying conditions and medically necessary surgeries.
Is IVF covered under maternity or standard health insurance plans?
IVF is typically excluded from both maternity and standard health insurance plans unless specifically mentioned in the policy.
Do insurer require medical proof or diagnosis for IVF coverage?
Yes, insurers usually require medical reports and a confirmed diagnosis before approving any fertility-related claims.
Are diagnostic tests for infertility included in insurance coverage?
Some plans cover tests like ultrasounds, hormone panels and semen analysis, depending on policy terms.
What are the common exclusions in infertility or IVF insurance?
IVF cycles, assisted reproductive procedures, fertility drugs and repeated treatment attempts are commonly excluded.
Does insurance cover multiple IVF cycles or only the first attempt?
When covered, insurance usually applies to a limited number of cycles with strict financial caps.
Are there any special infertility insurance plans or riders available in India?
A few insurers and corporate group policies offer fertility riders with partial coverage, waiting periods and specific eligibility conditions.