Disclaimer: This article is for informational purposes only and should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for any medical concerns.

Monsoons are notorious for bringing a plethora of diseases along with relief from the summer. Humidity and warm climate are the most ideal conditions for fungi to grow and spread infections - which is common across India, especially during monsoons.
In a recent study, “The burden of serious fungal infections in India”, it was stated that around 57 million Indians are affected by fungal infections each year. Although fungal infections are generally not fatal, some serious fungal infections can lead to uncertainties for people with weak immune systems, and hence, it is important to understand the most common fungal infections during the rainy season, what causes them, and how we can avoid them.
What Is a Fungal Infection?
A fungal infection, or mycosis, is a health condition caused by certain types of fungi entering and growing inside the body. These fungi are tiny living organisms commonly found in soil, plants, water, and even on our skin, and thrive in humid, warm climates. While many fungi are harmless, some can cause infections, especially when they grow in places where the body’s defences are weaker. Fungi usually enter the body through the air we breathe, through small cuts on the skin, or through contact with contaminated surfaces. They tend to grow in warm, damp areas, which is why infections often appear on the skin, nails, lungs, mouth, or private parts.
Common Types of Fungal Infections
Fungal infections range from mild conditions like athlete’s foot to serious systemic infections like Candidemia or Mucormycosis, especially in vulnerable individuals. Here are common types of fungal infections, the body parts they affect and which fungus causes the infection - especially prevalent in monsoon:
| Type of Fungal Infection | Commonly Affects | Fungus |
|---|---|---|
| Athlete’s Foot (Tinea Pedis) | Feet (especially between toes) | Trichophyton species |
| Ringworm (Tinea Corporis) | Skin (body, arms, legs) | Trichophyton, Microsporum |
| Candidiasis (Yeast Infection) | Mouth, throat, vagina, skin | Candida albicans |
| Nail Fungus (Onychomycosis) | Fingernails or toenails | Trichophyton rubrum |
| Jock Itch (Tinea Cruris) | Groin and inner thighs | Epidermophyton floccosum |
| Tinea Versicolor | Upper back, chest, neck | Malassezia furfur |
Athlete’s Foot
Ringworm
Candidiasis
Nail Fungus
Jock Itch
Tinea Versicolor
Also known as Tinea Pedis or “पैरों का दाद or Pairon ka Daad in Hindi, Athlete’s Foot is a common fungal infection that targets the feet, especially between the toes. It is caused by fungi such as Trichophyton rubrum, which thrive in moist and warm climates like monsoons. It often leads to itching, peeling skin, and sometimes painful cracks. In India, this infection frequently coexists with other tinea infections, particularly in humid states, and is increasingly common among young adults and athletes.
Ringworm, medically known as Tinea Corporis, and often referred to as “Daad or दाद ”, presents as circular, red, scaly patches on the skin. Despite its name, it’s not caused by a worm but by fungi like Trichophyton and Microsporum. It spreads through direct skin contact or contaminated surfaces. In India, tinea corporis is the most reported dermatophyte infection, accounting for nearly 39% of all fungal skin infections in dermatology clinics. (Study conducted on cumulative cases from 1939-2021).
Candidiasis, sometimes called a Yeast Infection, is caused by Candida albicans, a type of yeast that normally lives in small amounts on your skin or in your mouth and gut. It can cause infections when the balance is disturbed, typically showing up in the mouth (thrush), vaginal area, or skin folds. In India, invasive candidiasis affects an estimated 1.8 lakh Indians annually, especially in hospital settings or among immunocompromised individuals. (Study on Burden of Serious Fungal Infections in India).
Known as Onychomycosis, this fungal infection affects toenails and fingernails, making them thick, yellow, and brittle over time. It often starts as a white or yellow spot under the nail tip and gradually spreads. It is caused by fungi like Trichophyton rubrum and Candida. Indian studies report a prevalence ranging from 0.5% to 5%, particularly among those with diabetes or prolonged exposure to water.
Jock Itch, medically referred to as Tinea Cruris and locally known as "कमर का दाद or Kamar ka Daad”, is a red, itchy rash that affects the groin, inner thighs, and buttocks. It is more common in men and is often triggered by tight clothing, sweating, and lack of air circulation. The infection is caused by fungi like Epidermophyton floccosum. In Indian clinics, it accounts for up to 62% of tinea cases, especially in warm and tropical regions.
Also called Pityriasis Versicolor, this fungal skin condition causes small discoloured patches - either lighter or darker than your normal skin tone, which are mainly on the chest, back, and shoulders. Caused by the yeast Malassezia, which lives on healthy skin, it becomes problematic in hot and humid climates when it overgrows.
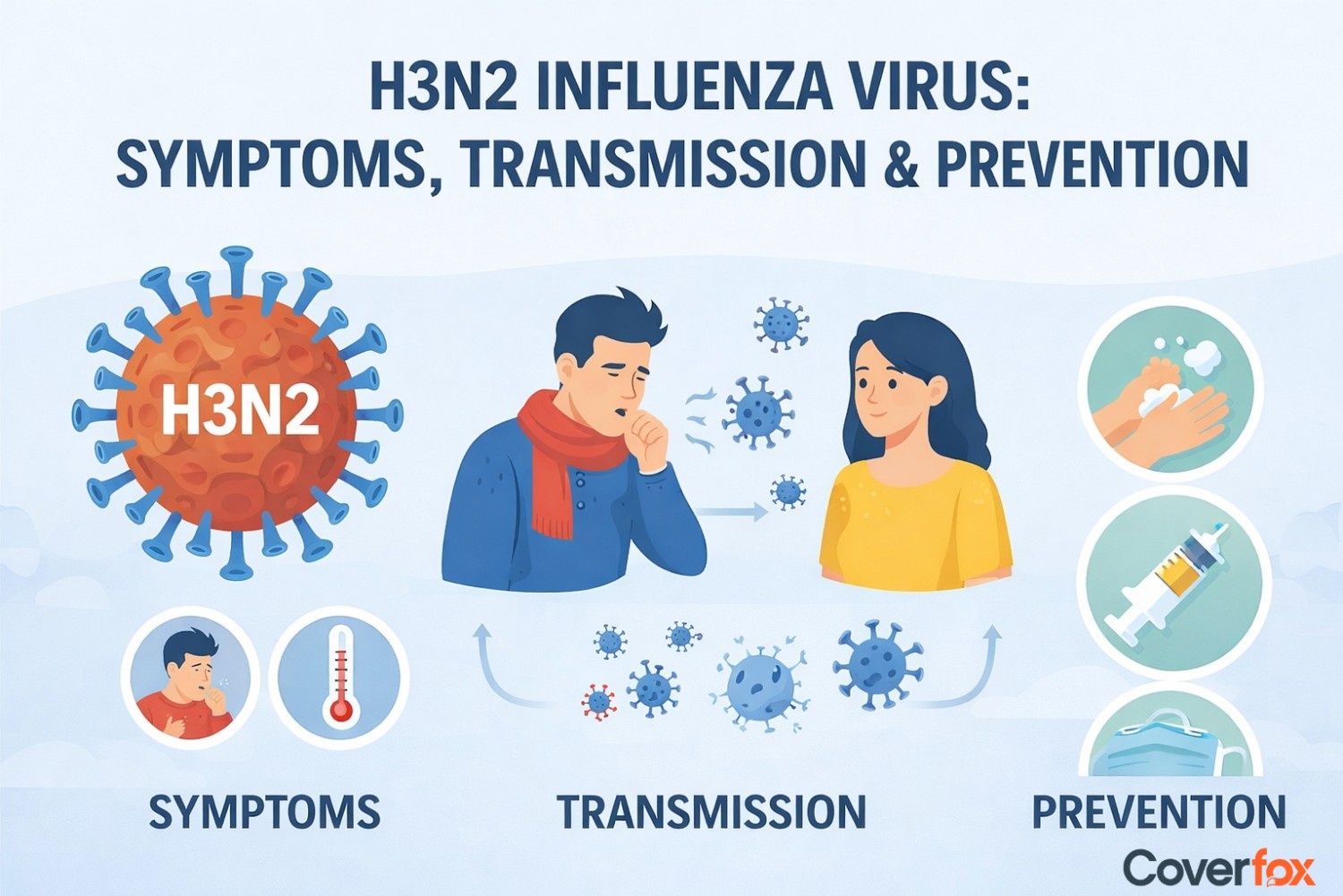
Symptoms of Fungal Infections
Fungal infections can be different based on the type, severity, and the part of the body affected. While some remain superficial, others may become invasive and systemic. Spotting the symptoms early can help you seek timely treatment.
Asthma-like symptoms
Fatigue
Headache
Muscle aches or joint pain
Night sweats
Weight loss
Chest pain
Itchy or scaly skin
Fungal spores can irritate the respiratory tract, causing wheezing, coughing, or shortness of breath, similar to asthma, especially in people with weakened immune systems or lung conditions.
Persistent tiredness is often associated with systemic fungal infections, as the body uses more energy fighting off the infection.
Fungal infections like sinus mycosis or fungal meningitis can cause headaches, particularly when the sinuses or brain are involved.
Some deep fungal infections cause body aches or joint discomfort, especially if the infection has spread beyond the skin.
Systemic fungal infections may cause fever and sweating at night, a sign that the body is trying to regulate its temperature while fighting infection.
Ongoing infections can lead to unintended weight loss due to appetite loss, malabsorption, or general illness.
In pulmonary fungal infections, chest pain can occur due to inflammation in the lungs or pleura (the lining around the lungs).
One of the most common signs of fungal infections, especially on the skin, scalp, or feet, includes persistent itching, flaking, or discoloured patches.
Why Fungal Infections Spike During Monsoon?
Monsoons are the perfect climate for fungal infections to rise. Warm climate, along with humidity, are the key culprits here. Due to the perfect environment created by constant moisture, warmth, and high humidity, fungi thrive and multiply rapidly on human skin, clothes, and even in the air. Here are the key reasons for Fungal inspection spikes during monsoon:
Increased Humidity
Wet Clothes & Footwear
Poor Ventilation
Contaminated Water
Weakened Immunity
The damp atmosphere provides ideal conditions for fungal growth, especially on sweaty or wet skin and clothing.
Wearing damp clothes or shoes for extended periods increases the risk of fungal infections, particularly on the feet, groin, and underarms.
Closed windows and minimal sunlight in monsoon restrict airflow, keeping areas like bathrooms and bedrooms damp, encouraging mould and mildew growth.
Walking through puddles or using unclean water can lead to fungal infections on the feet or nails.
Sudden weather changes can weaken the body’s immune response, making it easier for fungal spores to take hold and spread.
How to Prevent Fungal Infections in the Rainy Season?
We have to be extra careful during the rains and must protect ourselves against the potential threat posed by fungal infections. During rains, these diseases have a huge spike, and if not careful, can lead to infections that will irritate and cause great discomfort. Here’s how you can prevent fungal infections to some extent in the rainy season:
Personal Hygiene Tips
- Bathe daily with antibacterial or antifungal soap.
- Dry skin folds thoroughly after showering.
Clothing & Footwear Tips
- Wear dry, breathable clothes made of cotton.
- Change wet clothes or socks immediately.
Antifungal Products
- Apply antifungal powder in high-sweat areas.
- Use medicated creams if prone to infections.
Foot Care
- Wash and dry feet properly, especially between toes.
- Avoid walking barefoot in public wet areas.
Avoiding Cross-Contamination
- Do not share towels, shoes, or clothing.
- Wash and dry laundry thoroughly.
Disinfecting Shared Spaces
- Clean bathrooms with antifungal cleaners regularly.
- Keep rooms well-ventilated and dry.
Other Preventive Measures
- Boost immunity through a healthy diet.
- Use talcum powder in moisture-prone areas.
Treatment Options for Fungal Infections
If you are infected with a fungal infection, getting treatment at the earliest is your best option. Delaying treatment can lead to the severity of symptoms and, in worst cases, death. Here are the common treatments for fungal infections available:
Topical Antifungal Creams/Ointments
Oral Antifungal Medications
Antifungal Powders and Sprays
Specialised Treatments for Nails (Nail Lacquers)
Home Remedies (with medical supervision)
As your immediate measure, applying creams and ointments depending on the type of fungal treatment on the infected area is your first line of defence. They help reduce itching, inflammation, and stop fungal growth.
If topical ointments do not work, oral antifungal medications are used if the condition worsens. These are usually prescribed for skin, nail, or systemic fungal issues.
Ideal for preventing recurrence in sweaty or moist areas like feet and underarms. They help keep skin dry and inhibit fungal growth.
Medicated nail lacquers or paints are specifically designed to penetrate thick nails and treat fungal infections over time.
Natural solutions like diluted tea tree oil, apple cider vinegar soaks, or turmeric paste may help in mild cases, but should always be used with professional guidance.
Home Remedies for Common Fungal Infections During the Rainy Season
If you know what you are doing, and are acquainted with the particular type of fungal disease, certain home remedies can come in handy.
Disclaimer: If the wrong ointment is applied, it can lead to further irritation, itching and discomfort. These remedies are for mild cases only. Consult a doctor before using any ointment to prevent further damage.
Tea tree oil (diluted)
Apple cider vinegar soak
Turmeric paste
Neem leaves bath
Aloe vera gel
Coconut oil
Garlic paste
Natural antifungal that helps reduce itching and inflammation.
Creates an acidic environment that discourages fungal growth.
Contains curcumin with antifungal and anti-inflammatory properties.
Known for antifungal and antibacterial benefits.
Soothes irritated skin and may slow fungal activity.
Has mild antifungal action and moisturises dry, infected areas.
Contains allicin, which may help combat fungal pathogens.
Insurance Coverage for Fungal Infections
If you visit a doctor for a fungal infection, the immediate remedy the doctor may give you is an antifungal cream or ointment. However, in severe cases or if the patient has a weakened immune system, a viral or fungal infection is a dangerous threat, and in such severe cases, the doctor can advise having the infected mass surgically removed, which would require hospitalisation and medical costs. If you do not have health insurance, these costs will be out-of-pocket expenses. To avoid this, medical or health insurance is absolutely essential. It will cover any diagnostic tests, hospitalisation charges, surgical charges, etc as per the health insurance policy. Ensure your health insurance covers fungal diseases and read all policy-related documents carefully.
Wrapping Up
We must be careful of our health and our surroundings, especially during monsoons. Fungal infections are quite common in the season of rains, as it serves as a perfect ground for fungi to grow - because of humidity and warm climate. Fungal infection causes irritation, itchiness and discomfort and can be avoided with proper hygiene and cleanliness, and if you do get infected, general ointments do the work flawlessly. If the issue persists, do not delay in going to the doctor, as early treatment is necessary for fast recovery. Ensure you have health insurance to avoid unexpected expenses, and your policy has fungal infection coverage.
Also Read:
Frequently Asked Questions
Do fungal infections occur in humid weather?
Yes, humid weather creates the perfect environment for fungi to grow, especially in moist areas of the skin.
Are fungal infections contagious?
Many fungal infections are contagious and can spread through direct skin contact or sharing personal items like towels or footwear.
Can stress cause fungal infections?
Indirectly, yes. Stress can weaken the immune system, making the body more vulnerable to fungal infections.
Is salt water good for fungal infections?
Mild saltwater soaks may help dry out infected areas and reduce itching, but they aren’t a substitute for antifungal treatments.
Why are fungal infections itchy?
Fungal infections trigger an immune response that leads to inflammation, causing itching, redness, and discomfort.
What is the skin infection during monsoons?
Common skin infections include athlete’s foot, ringworm, and candidiasis, all of which are caused by fungi thriving in damp conditions.
Why is fungus mostly seen in the rainy season?
The rainy season increases moisture in the air and on the skin, promoting fungal growth, especially in sweat-prone areas.
.webp)
 in Insurance.webp)