Oral cancer is the abnormal growth of cells in the mouth, affecting the lips, tongue, gums, inner cheeks, or the lining of the throat. It often starts as a painless sore, lump, or red/white patch that does not heal. Major causes include tobacco use, alcohol consumption, and HPV infection. In India, oral cancer accounts for around 30% of all cancer cases, making it one of the most common cancers in the country, compared to about 5% globally (National Oral Cancer Registry). Early detection and timely treatment can significantly improve survival and recovery outcomes.
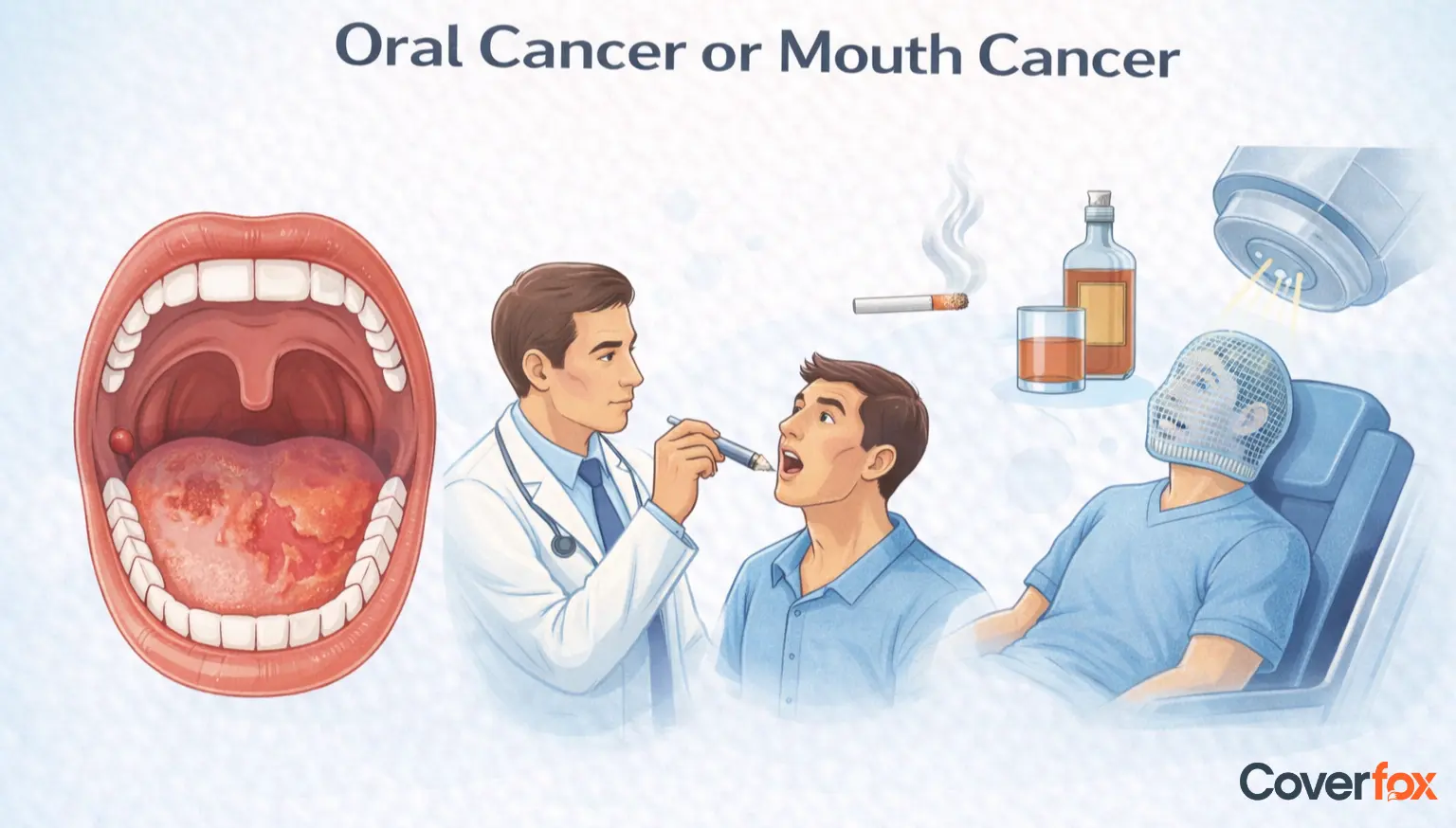
Mouth (oral) cancer develops due to a combination of lifestyle habits, infections, and long-term exposure to certain risk factors that damage the cells of the mouth.
Tobacco use in any form, including smoking and chewing
Excessive alcohol consumption, especially when combined with tobacco
Infection with human papillomavirus (HPV), particularly HPV-16
Chewing betel nut or areca nut, with or without tobacco
Excessive sun exposure to the lips
Poor diet lacking fruits and vegetables
Poor oral hygiene and chronic irritation from sharp teeth or ill-fitting dentures
Family history of cancer
Increasing age, especially above 40 years
Mouth cancer often starts with subtle changes that may not cause pain initially, which is why paying attention to persistent symptoms is important.
A sore, ulcer, or lump in the mouth or on the lips that does not heal within two weeks
Red or white patches inside the mouth or on the tongue
Persistent mouth pain, tenderness, or numbness
Difficulty chewing, swallowing, or speaking
Unexplained bleeding in the mouth
Changes in voice or persistent hoarseness
Loose teeth or dentures that suddenly stop fitting properly
Swelling in the jaw or neck area
Unexplained weight loss or ongoing fatigue
Oral cancer is classified based on the type of cells where the cancer begins. While several types exist, some are far more common than others.
This is the most common type of oral cancer and develops in the flat, thin cells that line the mouth, tongue, and throat. It tends to grow and spread faster than other types, but when detected early, treatment outcomes are generally good.
This is a rare, slow-growing form of oral cancer that usually appears as a thick, warty growth. It spreads very slowly and rarely moves to other parts of the body, so the prognosis is usually better when treated in time.
Oral cancer is diagnosed through a combination of clinical examination and medical tests that help confirm the disease and assess its spread.
A dentist or doctor visually examines the mouth, tongue, gums, and throat and feels for lumps or abnormal areas in the mouth and neck.
If a suspicious sore, patch, or lump is found, a small tissue sample is taken and tested to confirm whether cancer cells are present.
Scans such as CT, MRI, or PET scans are used to determine the size of the tumour and check whether the cancer has spread to nearby tissues or lymph nodes.
Oral cancer is staged based on the size of the tumour, lymph node involvement, and whether it has spread to other parts of the body. Staging helps doctors decide the best treatment and understand the prognosis.
The cancer is small and limited to one area of the mouth, with no spread to lymph nodes. Treatment at this stage is usually highly effective.
The tumour is larger but still confined to the mouth, with no lymph node involvement. Cure rates remain good with timely treatment.
The cancer may have spread to nearby lymph nodes or grown deeper into surrounding tissues. Treatment becomes more intensive at this stage.
The cancer has spread extensively within the mouth, to lymph nodes, or to distant organs. While more challenging to treat, therapy focuses on control, symptom relief, and improving quality of life.
Treatment for oral cancer depends on the stage of the disease, the size and location of the tumour, and the patient’s overall health. Often, more than one treatment approach is used to achieve the best outcome.
Surgery is the most common treatment for oral cancer, especially in early stages. It involves removing the tumour along with a margin of healthy tissue to ensure no cancer cells are left behind. In advanced cases, nearby lymph nodes in the neck may also be removed. Reconstructive surgery may be required to restore appearance and functions such as speech and swallowing.
Radiation therapy uses high-energy rays to destroy cancer cells. It may be used alone in early-stage cancers or after surgery to eliminate any remaining cancer cells. In advanced stages, radiation is often combined with chemotherapy. Side effects can include mouth sores, dry mouth, and difficulty swallowing, which are managed with supportive care.
Chemotherapy uses anti-cancer drugs to kill or slow the growth of cancer cells. It is usually recommended when oral cancer has spread or when combined with radiation (chemoradiation) to improve treatment effectiveness. Chemotherapy affects the whole body and may cause side effects such as fatigue, nausea, and lowered immunity.
Targeted therapy works by attacking specific molecules involved in cancer cell growth while causing less damage to normal cells. These treatments are often used in advanced or recurrent oral cancer and may be combined with radiation or chemotherapy to improve results.
After treatment, patients may need speech therapy, nutritional support, and dental care to help regain normal function. Emotional and psychological support is also an important part of recovery.
Oral cancer can be largely prevented by reducing exposure to known risk factors and maintaining good oral and overall health.
Avoid all forms of tobacco, including smoking and chewing
Limit alcohol consumption
Do not chew betel nut or areca nut
Maintain good oral hygiene and regular dental check-ups
Eat a balanced diet rich in fruits and vegetables
Protect lips from excessive sun exposure
Practice safe sex to reduce the risk of HPV infection
Seek early medical advice for any persistent mouth sores or changes
Anyone who notices persistent mouth sores, lumps, red or white patches, chronic pain or numbness, difficulty chewing or swallowing, unexplained bleeding, or voice changes should consult a dentist or doctor without delay. Even symptoms that seem minor or painless should not be ignored if they last for more than two weeks.
Early medical evaluation helps detect oral cancer at a more treatable stage, improves recovery outcomes, and can prevent complications. Having the right health insurance ensures timely access to diagnosis, treatment, and follow-up care, making prompt action a crucial step in protecting your health and financial well-being.
Oral cancer prognosis varies widely depending on how early the disease is detected and treated. When diagnosed at an early stage, survival rates can be much higher — with many studies showing that early-stage oral cancers (Stage I/II) have 5-year survival rates of around 80–90%. (Research on Early Detection of Oral Cancer)
Overall survival rates are lower when oral cancer is diagnosed at more advanced stages, making early detection, prompt treatment, and regular screenings crucial for improving outcomes. Factors that influence prognosis include the stage at diagnosis, general health of the individual, treatment type, and timely access to care. (Research on Survival Rate of Oral Cancer Patients in Kerala, India)
Reconstruction and rehabilitation play a vital role in helping patients regain function, appearance, and quality of life after oral cancer treatment. Surgical reconstruction may be required to repair areas affected by tumour removal, using tissue grafts or flaps to restore the structure of the mouth, jaw, or face. Dental restoration and prosthetics help replace missing teeth or jaw segments, improving chewing, speech, and facial balance.
Rehabilitation also includes speech and swallowing therapy to help patients relearn essential functions affected by surgery or radiation. In addition, psychological and emotional support is crucial to address anxiety, self-image concerns, and recovery-related stress. Successful recovery relies on a multidisciplinary healthcare team involving surgeons, dentists, speech therapists, oncologists, nutritionists, and counsellors working together to support long-term healing and well-being.
Living with oral cancer involves ongoing care, lifestyle adjustments, and emotional support to help patients maintain comfort, confidence, and quality of life after diagnosis and treatment.
Managing treatment side effects such as mouth dryness, pain, fatigue, or difficulty swallowing with medical guidance
Focusing on proper nutrition through soft, balanced, and high-protein diets to support healing
Maintaining good oral hygiene and regular dental care to prevent infections and complications
Attending scheduled follow-up visits for monitoring, early detection of recurrence, and rehabilitation support
Seeking emotional, psychological, and social support from healthcare teams, family, or support groups
Disclaimer: The information provided above is for general awareness and educational purposes only. It should not be considered a substitute for professional medical advice, diagnosis, or treatment.
Stage 1 mouth cancer is an early stage where the tumour is small and confined to one area of the mouth, with no spread to lymph nodes. Treatment at this stage is usually highly effective.
Common signs include a non-healing mouth sore, a lump or thickened area, red or white patches, persistent mouth pain or numbness, and difficulty chewing or swallowing.
Yes, oral cancer is treatable, especially when detected early. Treatment may include surgery, radiation, chemotherapy, or a combination of these approaches.
Life expectancy depends on the stage at diagnosis and response to treatment. Early-stage oral cancer has high survival rates, while advanced stages require more intensive care.
Oral cancer often starts as abnormal cell changes in the mouth, appearing as painless sores, lumps, or red or white patches that gradually grow if untreated.
A mouth sore or patch that does not heal within two weeks is a major red flag and should be checked by a dentist or doctor.
Regular self-checks of the mouth, routine dental visits, and prompt attention to persistent symptoms help in early detection.
The 2-week rule suggests that any unexplained sore, lump, or symptom lasting more than two weeks should be medically evaluated.
You should be concerned if symptoms like mouth sores, pain, bleeding, or difficulty swallowing persist or worsen over time.
Oral cancer can affect eating, speaking, and breathing, and in advanced stages, it may spread to lymph nodes or other organs.
Yes, smoking and other forms of tobacco use are among the strongest risk factors for oral and mouth cancers.



























